

|
Clinical Cases |
|
Pericardial Effusion
Similar to how a pleural effusion is an abnormal accumulation of fluid in the pleural space around the lungs, a pericardial effusion is an abnormal accumulation of fluid in the pericardial sac surrounding the heart. The fluid of a pericardial effusion can be number of different things:
- Transudative - A transudate is an extravascular fluid that is low in protein, is generally acellular, and occurs in a non-inflammatory setting. It results from either an increase in hydrostatic pressure or a decrease in osmotic pressure inside blood vessels. A transudative pericardial effusion could occur in the setting of CHF (congestive heart failure- increased hydrostatic pressure in venous system as heart begins failing to push blood into the arterial system) or nephrotic syndrome, in which the kidneys leak massive amounts of protein resulting in hypoalbuminemia and so decreased osmotic pressure in the blood vessels.
- Exudative - In comparison to a transudate, an exudate is an extravascular fluid that is seen in a setting of inflammation. There are many types of exudates with varied compositions. A pericardial effusion caused by an exudate is called a pericardial empyema, and most commonly occurs in the setting of infection.
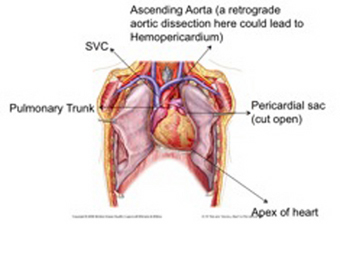
- Hemorrhagic - When blood leaks into and fills the pericardial sac, it is called a hemopericardium. Most commonly this is caused by trauma, but it can also be caused by retrograde dissection of the ascending aorta. An aortic dissection is when the tunica intima of the aorta tears, allowing blood to flow into the tunica media and split the media between the internal and external elastic laminae. This separation of the aortic wall, or aortic dissection, can move anterograde toward the iliac bifurcation or retrograde toward the aortic root. If the dissection occurs in the ascending aorta and moves retrograde, it can eventually lead to rupture of the aortic wall inside the pericardial sac, creating a massive hemopericardium.
- Malignancy - A fluid secreting malignancy could also be the cause of a pericardial effusion.
Cardiac Tamponade
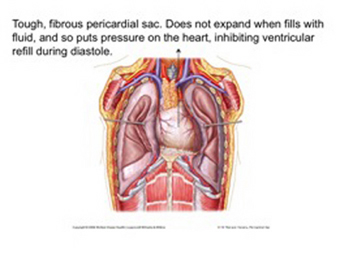
The pericardial sac is a tough, fibrous structure that normally holds about 25-50 cc of fluid around the heart. As fluid begins building up to an abnormally high level in the pericardial sac, the sac resists stretching and so puts pressure in the heart. After 150-250 cc of fluid has accumulated, a condition known as cardiac tamponade occurs. Cardiac tamponade is an emergency medical condition in which the fluid build-up in the pericardial sac exerts enough pressure on the heart to prevent refilling of the ventricles during diastole. This results in low stroke volume, low cardiac output, and eventually shock as the body enters a hypoperfusional state. Symptoms of cardiac tamponade are similar to those seen in shock. Classic cardiac tamponade presents 3 signs known as Beck's triad:
- Hypotension - due to decreased stroke volume
- Jugular venous distension - due to reduced venous return to the heart
- Muffled heart sounds - due to the muffling effect of fluid surrounding the heart
Pericardial Effusion on CT
The image below is called a CTA (CT Angiography) scan, and is created by taking a CT scan of someone after a contrast dye has been injected into their circulatory system. Notice in this scan how blood containing the contrast appears as radiopaque as bone. As you can see, the heart in this patient is surrounded by a halo of fluid. The black space seen between the heart and the effusion is pericardial fat lying on the surface of the heart.
The movie below is the CT scan of cadaver 33492. Begin looking at the scan by familiarizing yourself with the heart, using the ascending aorta (time= 53, K9, very collapsed) to find the left ventricle, the SVC (time= 50, J10) to find the right atrium, the pulmonary trunk (time= 52, L9) to find the right ventricle, and the pulmonary veins (time= 56, J11 and M12) to find the left atrium. Now look at the heart from time 50-60, noting how its chambers are surrounded first by a ring of black (normal pericardial fat) and then by a thick ring of gray. This thick outer ring of gray is all fluid that has accumulated in the pericardial sac. It is most prevalent around the left ventricle at time= 55-60, N9.
This patient's pericardial effusion has forced other structures out of their normal orientation in the body. For example, notice how the trachea (time= 45-50, K9) deviates to the right once inside the chest. This is due to the enlarged heart crowding into the superior mediastinum and pushing the trachea away from midline. Also notice how the right kidney (comes into view at time= 65, I12) is seen to be higher in the body than the left kidney (comes into view at time= 67, N12). Normally, the liver pushes the right kidney down below the level of the left kidney, but in this patient the greatly enlarged heart is forcing the left kidney below the level of the right kidney.
Treatment
Caring for someone with a pericardial effusion that is causing cardiac tamponade requires the support resources of a hospital. The patient's shock is managed until a procedure can be performed to remove the fluid from around the heart (i.e. giving oxygen to the patient and vasopressors to combat the systemic vasodilation and subsequent hypotension that is characteristic of shock). Removal of the fluid in the pericardial sac is done by pericardiocentesis. This procedure involves inserting a needle, usually under ultrasound guidance, into the pericardial sac and aspirating fluid from the sac. As you can see in the image below, the best place to insert the needle for a pericardiocentesis is along the left sternal border in the 5th intercostal space. The cardiac notch of the left lung creates a bare area of the pericardial sac at this point, giving direct access to the heart. Not only is the pericardial sac unobstructed by the lung at this point, but it is also near the apex of the heart, where fluid is most likely to accumulate.