|
Clinical Cases |
|
Pleural Effusion
The pleurae are two serous membranes that each forms a sac in the thorax. Like a fist pushing into a loosely inflated balloon, the lungs embed themselves in the pleurae so that they are surrounded by, but not contained within, the pleurae. This creates two different surfaces to the pleurae: the lining of the inner thoracic wall (parietal pleurae), and the lining of the lung itself (visceral pleurae). There are also two pleural recesses that do not have lung embedded in them: the costodiaphragmatic and costomediastinal recesses. In between the visceral and parietal pleurae is a potential space (this is the space within the pleural sac- inside the loosely inflated balloon). This pleural space normally contains 2-10 cc of fluid. There is a tremendous amount of fluid turn over taking place between the two pleural surfaces. It is thought that as much as 100 cc of fluid is produced each hour at the parietal pleurae, which is then drained by the visceral pleurae and lymphatics. Pleural effusions occur when there is dysfunction in the production or drainage of fluid in the pleural space.
Similar to other types of effusion (pericardial effusion, abdominal effusion- ascites), pleural effusions can be composed of a number of different fluid types:
- Transudative effusion (Hydrothorax): These are caused by either an increase in intravascular hydrostatic pressure or a decrease in intravascular oncotic (colloid osmotic) pressure. A transudate occurs in a non-inflammatory setting, and typically results from systemic factors that alter the production or absorption of pleural fluid. Congestive heart failure, especially failure of the left ventricle, can result in a pleural effusion via increased intravascular pressure. Hypoalbuminemia (as a result of nephrotic syndrome, for example) can result in pleural effusion via decreased intravascular oncotic pressure.
- Exudative effusion (pyothorax or empyema): These typically result from infectious or neoplastic diseases involving the pleura. Exudative effusions occur in inflammatory settings and typically result from local factors that alter the production or drainage of pleural fluid. Most common causes of exudative pleural effusion are bacterial pneumonia, cancer (lung cancer, breast cancer, and lymphoma most typical), viral pneumonia, and pulmonary embolism.
- Hemorrhagic effusion (hemothorax): A hemothorax is an accumulation of blood in the pleural space. It is typically caused by blunt or penetrating trauma to the chest that results in rupture of the parietal or visceral pleura, which allows blood to enter the pleural space (if the trauma is penetrating and air is allowed to enter as well, this is called hemopneumothorax). As blood and/ or air fills the pleural space, the negative pressure in the pleural space relative to the lung is lost, and the lung can potentially collapse.
- Chyle effusion (chylothorax): Chyle is the fluid formed in the lacteals (lymphatic capillaries that absorb fats from small intestine) of the small gut, and it is composed of lymph and emulsified fats. This fluid can enter and accumulate in the pleural cavity if the thoracic duct, or a main contributing branch to it, is obstructed (i.e. lymphoma) or ruptured (trauma, iatrogenic injury).
Pleural Effusion On CT Scan
The image below on the left is a CT scan of a healthy chest at the T7 vertebral level. Notice how the lung spaces are clear all the way around the inner chest wall. The image to the right is the same CT scan viewed through the lung window. Notice on this image how healthy lung tissue is visible throughout the lung, with no fluid consolidations present.


The movie file below is a CT scan of cadaver 33472. Scan down to the T7 vertebral level (time= 55), and compare these lungs to those in the images above. Notice all of the gray shading (fluid appears gray on CT). This fluid nearly reaches the anterior edge of the vertebral bodies. CT scans are done with the patient lying in the supine position, and so any pleural effusion will spread out along the posterior aspect of the pleural space (as opposed to chest X-rays taken with the patient standing, in which pleural effusions tend to collect in the costodiaphragmatic recesses).
Treatment
If a pleural effusion is found it is important to try and determine the cause and type of effusion fluid present because treatment will vary from a strictly medical approach to a medical and surgical approach depending on the severity and cause of the effusion. A transudative effusion caused by congestive heart failure (CHF), for example, can usually be treated with diuretics and other medications used to treat CHF. Once the CHF is under control, the pleural effusion typically resolves. If the effusion is exudative or hemorrhagic, however, the fluid typically needs to be mechanically removed from the pleural space in addition to any medical treatment for the underlying cause. There are two techniques for removing fluid or air that is accumulating in the pleural space:
- Thoracocentesis: Under local anesthetic, a large hollow bore needle (cannula) is inserted into the costodiaphragmatic recess of an upright patient. The costodiaphragmatic recess is the lowest extent of the pleural sac, and so it is where any pleural effusion will collect in an upright patient.
As you can see in the image above, the costodiaphragmatic recess is in a different location depending on where you insert the needle. At the mid-clavicular line, the costodiaphragmatic recess is between ribs 6 and 8; at the midaxillary line it is between 8 and 10; and at the paravertebral line it is between 10 and 12. The image below depicts a typical thoracocentesis. Notice that the fluid is being collected in the image. This is because removing the fluid not only alleviates discomfort and improves ventilation for the patient, but analysis of the fluid almost always yields useful clinical information about the cause of effusion. 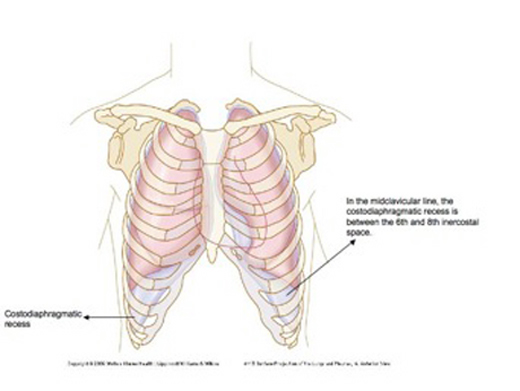

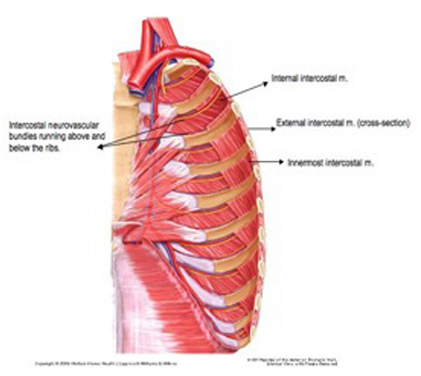
- Chest tube (Thoracostomy): An ostomy is defined as a surgically introduced hole in the body. A thoracostomy is, therefore, a surgically introduced hole in the thorax. A plastic chest tube is inserted into the hole, which then can be used as a drain for fluid and air that has entered the pleural space. Under local anesthetic and using a surgical sterile field, an incision is made in the chest wall at the level where the chest tube will be inserted. This incision should be made as central in the intercostal space as possible to avoid damaging the intercostal vessels and nerves that run along the superior and inferior borders of the ribs. A plastic chest tube is then inserted through this incision, past the skin and muscles of the chest wall (from superficial to deep in the axillary region: external intercostal mm., internal intercostal mm., innermost intercostal mm.). The image below to the left shows the pertinent anatomy of the chest wall, and the image on the right shows a typical chest tube set-up, with collection vesicle below the chest so that fluid drains out of the pleural space and not back into it (though one-way valves in the tubing also act to ensure no back flow into the pleural space).