

|
Clinical Cases |
|
Totally Implantable Venous Access System (Medical Port)
Totally implantable venous access systems (TIVAS) are a form of central venous access device that remains entirely under the skin. There are many different brand name devices in use, and the names of these devices are often used in place of the term TIVAS. Examples of these devices include PortaCath, MediPort, PassPort, and LifeSite (a device specifically designed for hemodialysis patients). For the purpose of this case, we will use the term "port".
How Ports Work
Ports consist of two main components: a reservoir with a self-sealing silicone septum for needle insertion, and a catheter that runs from the reservoir to the site of drug infusion. Ports are surgically inserted under the skin of the right upper chest. The catheter is surgically inserted into one of the main veins of the upper chest (subclavian v., internal jugular v., or superior vena cava). Ideally, the tip of the catheter is advanced to a point in the SVC just outside the right atrium.
The procedure is done under local anesthesia and sometimes conscious sedation. Because the entire port device is under the skin, patients can bathe and swim without risk of infecting the port site. When it is time for an infusion or blood draw, a needle specifically designed to fit the portal reservoir is inserted through the skin and through the self-sealing silicone septum. Negative pressure is pulled to withdraw blood back into the needle (this ensures the port is clear of obstructions), and then a saline flush is administered to clear the port. Drug is then infused and/or blood is drawn. After every infusion or blood draw, a small amount of heparinized saline is injected into the port to prevent clotting and to keep the port clear for the next use.Why Ports are Used
These devices are used in patients that require frequent venous infusions and/ or blood draws over a prolonged period of time. Cancer patients receiving long-courses of chemotherapy are the most common type of patient to receive a port. The benefits of a port for these patients are two fold:
- The port allows easy, frequent access to the patient's venous circulation with minimal infection risk and discomfort for the patient.
- When given peripherally, chemotherapeutics have been shown to cause a great deal of damage to veins. It is thought that many chemotherapeutics induce the venous endothelium to release interleukin-1, which in turn causes an increase in CAM (cellular adhesion molecule) expression on the endothelial surface. This makes the assaulted endothelium highly reactive to platelets, leading to large spread thrombosis and hardening of the vein at the site of chemotherapy infusion. For patients receiving many chemotherapy infusions, peripheral sites of venous access eventually become too damaged to use. By slowly infusing the chemotherapeutic agent through a port that leads directly to the SVC or right atrium, the chemotherapeutic is delivered to the patient's largest venous blood pool and so kept at a concentration low enough to minimize or prevent venous/ right atrial damage.
Ports on Plain Film and CT Scan
The image below is a chest X-ray of a patient with a port device. The reservoir is located on the right mid-clavicular line in the 4th intercostal space. The catheter can be seen running laterally from the reservoir toward the right axillary vein, and then curving back around medially to follow the right subclavian vein to the right brachiocephalic vein, finally ending in the SVC just outside the right atrium.
The image below is the scout film of cadaver 33450. Look at the right upper chest, just outside the shadow of the right lung. A small circle of high attenuation (increased radiopacity-whiteness) can be seen just below the clavicle on the right chest. This is the reservoir of a port this patient had put in prior to receiving chemotherapy for metastatic lung cancer.
Image courtesy of Pixman
Now look at the movie file below, which is the CT scan of the same cadaver. Scan down to the chest, paying special attention to the superficial right chest wall. At time= 52, H7, you should see the port's reservoir just beneath the patient's skin. Continue scanning up and down to follow the catheter (in this patient, the catheter loops up and over the right clavicle, and so to follow the catheter in successive cross-sections, you will have to scan up first and then down). Start following the catheter coming off the reservoir at time= 51. Notice how the catheter loops up and over the right clavicle (time= 48) before entering the right internal jugular vein (time= 49, J9). From here, the catheter can be seen following the internal jugular vein to the right brachiocephalic, and then finally the SVC, where the catheter terminates just outside the right atrium.
Other types of Venous Access Systems
Another commonly used central venous access device is the Peripherally Inserted Central Catheter line, known simply as a PICC line. These devices do not exist entirely underneath the skin, and so extra caution must be taken to avoid infection at the site of access to the catheter. As the name suggests, PICC lines are inserted into peripheral veins such as the cephalic, basilic, or brachial veins of the arm. The catheters are then thread proximally toward the cavoatrial junction (where the SVC empties into the right atrium). PICC lines are usually used for drug regimens that last 30 days or less. If PICC lines are left in for longer than 30 days, risk of complications like catheter occlusion, thrombosis, thrombophlebitis, and infection increase.
The chest film shown below is of a patient with a PICC line inserted in what appears to be the left basilic vein. See if you can follow the catheter all the way from the left arm, through the axilla, across the chest in the left subclavian and brachiocephalic veins, and finally ending just outside the right atrium in the SVC.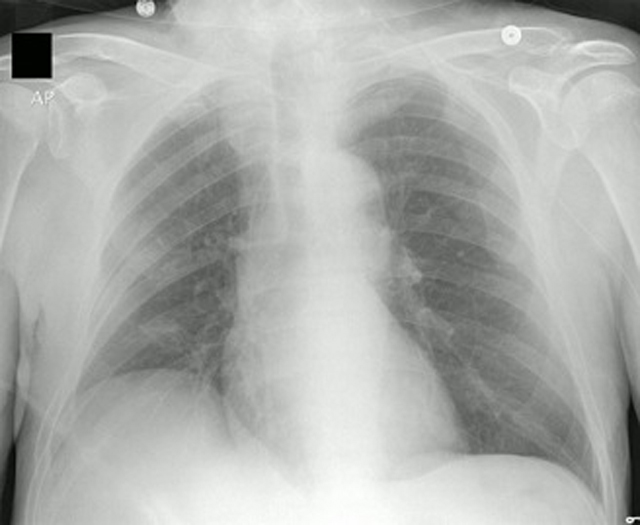
Image courtesy of OctavioL