

|
|
||||||||||||
Dissector Answers - Rectum, Anal Canal, & Pelvic Floor |
|||||||||||||
Learning Objectives:
Upon completion of this session, the student will be able to:
- Recognize the features of the rectum that differentiate it from the colon.
- Describe the point at which the anal canal begins.
- Describe the internal features of the anal canal, and determine the point at which its lining changes from cutaneous to mucosal.
- Recall the lymph node groups that drain the rectum and anal canal.
- Organize blood and nerve supply to the rectum and anal canal.
- Describe the formation of the two sciatic foramina. List the muscles, nerves, and vessels which pass through each.
- Demonstrate the origins of the piriformis and obturator internus muscles and describe two specializations of the obturator fascia.
- Identify the pelvic diaphragm and differentiate its components.
- Demonstrate the formation of the sacral plexus, its relationship to the piriformis muscle and gluteal vessels, and its pelvic splanchnic nerves.
- Identify and describe the inferior hypogastric (pelvic) plexus and its connections to the superior hypogastric plexus via the hypogastric nerves.
- Identify and describe the sacral sympathetic trunks and the sacral sympathetic nerves.
- Trace the sympathetic and parasympathetic nerve supply to any pelvic organ, listing the location of the preganglionic cell body, the course of preganglionic fibers, the location of the postganglionic cell body, and the course of postganglionic fibers.
- Trace the skeletal and ligamentous boundaries of the perineum, and define the anal and urogenital triangles.
- Describe the position and boundaries of the ischioanal fossa.
- Describe the structure, contents, and course of the pudendal canal.
- Differentiate between the internal and external anal sphincters in structure and function.
Learning Objectives and Explanations:
1. Recognize the features of the rectum that differentiate it from the colon. (W&B 485, 535, N 307, 311, 360, 361, 393, 394, 409, 410, 412, TG 6-08A, 6-08B, 5-14, 6-15A, 6-15B, 6-15C, 6-16, 6-19A, 6-19B, 5-28)2. Describe the point at which the anal canal begins. (W&B 536-538, N 393, 394, 398, 399, 402, 406, 407, 408, 410, 411, TG 6-16, 6-17A, 6-17B, 6-19A, 6-19B, 5-28, 6-30, 6-33, 6-34)There are two differences visible from the outside. First, the lower one-third of the rectum has nothing to do with peritoneum, and its superior two-thirds is retroperitoneal to varying degrees. The sigmoid colon, on the other hand, is peritoneal throughout its length. Second, the pattern of the teniae coli changes as the transition from sigmoid colon to rectum occurs. The sigmoid colon, like the rest of the colon, has three longitudinal muscular bands. These coalesce into two bands, anterior and posterior, on the rectum.
On the inside, the rectum has side-to-side "waviness", due to transverse rectal folds, that is not present in the sigmoid colon.
3. Describe the internal features of the anal canal, and determine the point at which its lining changes from cutaneous to mucosal. (W&B 537-538, N 393, 394, 398, 399, 402, 406, 407, 408, 410, 411, TG 6-16, 6-17A, 6-17B, 6-19A, 6-19B, 5-28, 6-30, 6-33, 6-34)The anal canal begins where rectal ampulla narrows, which is at the level of a "U"-shaped sling formed by puborectalis muscle. As a result of this sling, the direction of the gut tube abruptly changes. While the distal rectum runs anteroinferiorly, the anal canal, deviating almost 90 degrees, runs posteroinferiorly.
Images from "Anatomy of the Human Body" by Henry Gray are provided by:
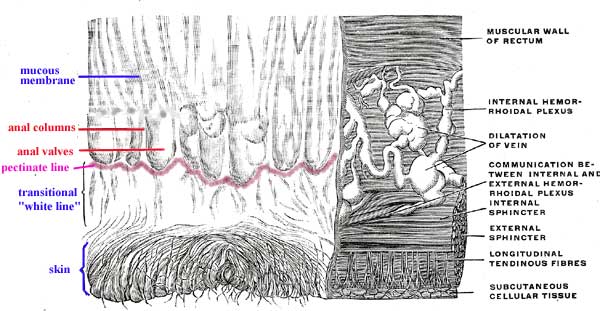
The lining of the anus officially changes from "skin" to mucosal at the pectinate line, though there is a transitional zone, or "white line", between the two areas. The pectinate line runs along the inferior borders of the anal valves, which are mucosal folds connecting the anal columns to one another.
4. Recall the lymph node groups that drain the rectum and anal canal. (W&B 535-538, N 266, TG 6-33, 6-34)5. Organize blood and nerve supply to the rectum and anal canal. (W&B 535-538, N 393, 394, 398, 399, 402, 406, 407, 408, 410, 411, TG 6-16, 6-17A, 6-17B, 6-19A, 6-19B, 5-28, 6-30)The lymphatic drainage of the rectum and anal canal mostly follows the blood vessels supplying the area. There are two primary paths for lymph leaving the area above the pectinate line:
- to the inferior mesenteric lymph nodes - efferent vessels from the upper rectum go to the inferior mesenteric lymph nodes, then to the lumbar nodes/trunk, finally ending in the thoracic duct/cisterna chyli.
- to the internal iliac lymph nodes - efferent vessels from the distal rectum go to the internal iliac and then common iliac lymph nodes, then to the lumbar nodes/trunk, finally ending in the thoracic duct/cisterna chyli.
Lymph from the cutaneous region of the anus, i.e. below the pectinate line, drains to the superficial inguinal lymph nodes. From there it goes to the external iliac and/or deep inguinal lymph nodes, then on to the common iliac lymph nodes, lumbar nodes/trunk, and thoracic duct (cisterna chyli).
6. Describe the formation of the two sciatic foramina. List the muscles, nerves, and vessels which pass through each. (W&B 570-571, N 352, 503, TG 3-28, 6-06)In addition to dividing the lymphatic drainage, the pectinate line also divides the arterial supply, venous drainage, and innervation of the anal canal. Superior to the pectinate line we have blood coming from the superior rectal artery, and draining to the portal system via the superior rectal veins, although distal rectum also drains to middle rectal veins and the internal iliac veins. Visceral afferent (pain and stretch) innervation of the rectum, unlike the rest of the GI tract above (which travels via its sympathetic supply), travels with its parasympathetic supply from the pelvic splanchnic nerves, S2-4. Inferior to the pectinate line we have blood coming from the inferior rectal arteries, draining into the caval system via the inferior rectal veins (this is an area of anastomosis between the two systems), and somatic (voluntary muscle, cutaneous sensory) innervation via the inferior rectal nerves, which happen to arise from S2-4 also, although it is important to note that they are not otherwise associated with the pelvic splanchnic nerves. Above pectinate line, lymphatics drain to inferior mesenteric and internal iliac nodes, whereas below pectinate line they drain to superficial inguinal nodes like the rest of the perineum.
7. Demonstrate the origins of the piriformis and obturator internus muscles and describe two specializations of the fascia of the latter. (W&B 564-565, N 367A, 367B, 369, 503, TG 3-28, 6-21A, 6-21B, 6-22)This is something that only makes sense in three dimensions. You must look at a pelvis from your bone box or in the lab, and figure out where these ligaments are going. Luckily, they are named in a very logical way. These anterior and posterior views might help.
Images from "Anatomy of the Human Body" by Henry Gray are provided by:
The sacrotuberal ligament connects the sacrum to the the ischial tuberosity. With the pelvis in the correct position, it runs mostly inferolaterally from the sacrum to the tuberosity, and only slightly anteriorly. The sacrospinal (sacrospinous) ligament connects the sacrum to the ischial spine. With the pelvis in correct anatomical position, it runs anterolaterally from the sacrum to the ischial spine, but does not deviate much in the superior-inferior axis.
These ligaments, along with the greater sciatic notch and the lesser sciatic notch, make up the greater sciatic foramen and the lesser sciatic foramen, respectively.
greater sciatic foramen: bounded anteriorly and superiorly by the posterior border of the hip bone (greater sciatic notch), posteriorly by the sacrotuberal ligament, and inferiorly by the sacrospinal ligament. The piriformis muscle passes through this opening, as do these nerves and vessels:
- superior to piriformis muscle: superior gluteal vessels and nerve
- inferior to piriformis muscle: inferior gluteal vessels and nerve, the sciatic nerve, the posterior femoral cutaneous nerve, and the nerve to the quadratus femoris muscle - also, the internal pudendal vessels and nerve and the nerve to the obturator internus muscle leave the pelvis via this opening, but enter the perineum through the lesser sciatic foramen (see below)
lesser sciatic foramen: bounded anteriorly by the ischial tuberosity, superiorly by the ischial spine and sacrospinal ligament, and posteriorly by the sacrotuberal ligament. It transmits the tendon of the obturator internus muscle - also, the nerve to the obturator internus muscle and the internal pudendal vessels and nerve, which left the pelvis via the greater sciatic foramen, re-enter the pelvis (in the case of the nerve to the obturator internus muscle) or the perineum (in the case of the internal pudendal vessels and nerve) via the lesser sciatic foramen
8. Identify the pelvic diaphragm and differentiate its components. (W&B 565-566, N 367A, 367B, 368, 369, 370, TG 6-23, 6-21A, 6-21B, 6-22, 6-23)The piriformis muscle takes origin from the anterior surfaces of S2 to S4, both between and lateral to the sacral foramina. It exits the pelvis via the greater sciatic foramen, inserting on the greater trochanter of the femur in order to rotate the thigh laterally. (Latin, piriformis = pear-shaped)
The obturator internus muscle takes origin from the whole bony rim of the obturator foramen, the inner surface of the obturator membrane, and a large area of the inner surface of the ischium. It leaves the pelvis (or, more correctly, its tendon does so) via the lesser sciatic foramen to insert onto the greater trochanter of the femur in order to rotate the thigh laterally. Its fascia has two specializations. First, there is a strong band that stretches between the spine of the ischium and the superior pubic ramus. This is the arcus tendineus levator ani, which gives origin to the levator ani muscles. The other specialization is the obturator membrane, which nearly covers the entire obturator foramen, only leaving space for the obturator nerves and vessels to exit.
9. Demonstrate the formation of the sacral plexus, its relationship to the piriformis muscle and gluteal vessels, and its pelvic splanchnic nerves. (W&B 559-561, N 402, 409, 410, 412, 415, 416, 417, 497, 499A, 499B, TG 3-25A, 3-25B, 6-17, 6-18, 6-19)The pelvic diaphragm is shaped like a bowl, with bony attachments at the pubic symphysis and the coccyx. Between those bones, it is attached to a thickening of the obturator internus muscle fascia called the arcus tendineus levator ani. It is made of two muscles, one of which is divided into 3 (or 4) parts.
Muscle Origin Insertion Action coccygeus ischial spine side of the coccyx and lower sacrum elevates the pelvic floor levator ani posterior surface of the body of the pubis, arcus tendineus levator ani, ischial spine anococcygeal raphe and coccyx elevates the pelvic floor iliococcygeus (part of levator ani) arcus tendineus levator ani and the ischial spine anococcygeal raphe and the coccyx elevates the pelvic floor pubococcygeus (part of levator ani) posterior aspect of the superior pubic ramis coccyx elevates the pelvic floor puborectalis (part of levator ani) posterior aspect of the body of the pubis unites with the puborectalis m. of other side posterior to the rectum draws the distal rectum forward and superiorly pubovaginalis (sometimes listed, part of levator ani) posterior aspect of the body of the pubis fascia of the vagina and perineal body draws the vagina forward and superiorly Furthermore, the diaphragm includes the inferior fascia and the superior fascia. The inferior fascia is an extension of the obturator internus fascia and is continuous with the fascia of the external sphincter ani muscle. The superior fascia is an extension of the transversalis fascia. The two layers are continuous in the urogenital hiatus.
10. Identify and describe the inferior hypogastric (pelvic) plexus and its connections to the superior hypogastric plexus via the hypogastric nerves. (W&B 562-564, N 409, 410, 412, TG 8-18, 8-19, 8-20, 8-21)Images from "Anatomy of the Human Body" by Henry Gray are provided by:
The sacral plexus proper includes contributions from L4 through part of S4. (Also shown here is the coccygeal plexus, which includes the rest of S4, S5, and the coccygeal nerve.) All of the contributing nerves, except S4, divide into anterior (shown yellow above) and posterior (shown yellow with black shading above) branches.
sciatic nerve: actually two separate nerves that are usually fused together (though in some cases they are not) - the tibial nerve, from anterior branches of L4 through S3, and the common fibular (peroneal) nerve, from the posterior branches of L4 through S2. The sciatic nerve runs under the piriformis muscle, emerging at its inferior border. It travels through the greater sciatic foramen, and on into the thigh. The sciatic nerve provides motor innervation to the hamstrings (posterior thigh muscles) and all of the muscles in the leg and the foot.
superior gluteal nerve: from posterior branches of L4 through S1. Travels through the greater sciatic foramen superior to the piriformis muscle, and moves laterally between the gluteus medius muscle and the gluteus minimus muscle. Provides motor innervation to gluteus medius muscle, gluteus minimus muscle, and tensor fascia lata muscle.
inferior gluteal nerve: from the posterior branches of L5 through S2. Travels through the greater sciatic foramen inferior to the piriformis muscle, and travels for a short distance deep to the gluteus maximus muscle but superficial to the sciatic nerve. It provides the sole motor innervation of the gluteus maximus muscle.
nerve to quadratus femoris muscle: from the anterior branches of L4 through S1. Travels through the greater sciatic foramen inferior to the piriformis muscle. Provides motor innervation to quadratus femoris and inferior gemellus muscles.
nerve to obturator internus muscle: from the anterior branches of L5 through S2. Travels through the greater sciatic foramen inferior to the piriformis muscle, but then loops back around to re-enter the pelvis through the lesser sciatic foramen. Provides motor innervation to the obturator internus and superior gemellus muscles.
posterior femoral cutaneous nerve: from the anterior branches of S2 and S3 and the posterior branches of S1 and S2. Travels through the greater sciatic foramen inferior to the piriformis muscle, and lies alongside the sciatic nerve. It provides sensory innervation to the skin of the back of the thigh in addition to the skin of the lower and lateral buttocks (through gluteal branches) and the perineum (via perineal branches).
pudendal nerve: from the anterior branches of S2 through S4. Travels through the greater sciatic foramen inferior to the piriformis muscle, but then loops back around to enter the perineum through the lesser sciatic foramen, entering the pudendal canal. Provides motor innervation to the muscles of the perineum, and is the primary sensory innervation to the genitalia. (Latin, pudere = to be ashamed)
perforating cutaneous nerve: from the posterior branches of S2 and S3. Pierces the sacrotuberal ligament to provide sensory innervation to the skin of the medial part of the fold of the buttock.
nerve to piriformis muscle: from posterior branches of S1 and S2. Provides motor innervation to the piriformis muscle.
nerves to coccygeus and levator ani muscles: from anterior branches of S3 and S4. Provide motor innervation to coccygeus and levator ani muscles.
pelvic splanchnic nerves: from the ventral primary rami of S2 through S4. Travel to the inferior hypogastric plexus (see below).
perineal branch of the fourth sacral nerve: from the anterior branch of S4. Descends through the coccygeus muscle and runs anteriorly to the external sphincter ani muscle. Provides motor innervation to this muscle and sensory innervation to the overlying skin.
11. Identify and describe the sacral sympathetic trunks and the sacral splanchnic nerves. (W&B 562-564, N 415, 416, 417, TG 8-18, 8-20)The inferior hypogastric plexus is a major meshwork of nerves that are located on either side of the rectum, cervix, and lateral vagina in the female, or on either side of the rectum, prostate, and seminal vessicles in the male. It receives the following:
hypogastric nerves: from the superior hypogastric plexus. These are the primary ways in which sympathetic neurons reach the hypogastric plexus, and therefore the pelvic viscera.
sacral splanchnic nerves: from the second and/or third ganglia of the sacral sympathetic trunk. These are the secondary ways in which sympathetic neurons reach the hypogastric plexus, and therefore the pelvic viscera.
pelvic splanchnic nerves: from the ventral primary rami of S2 through S4. These are the ways in which parasympathetic neurons reach the hypogastric plexus, and therefore the pelvic viscera and distal colon. (Remember that the parasympathetic part of the autonomic nervous system is the "craniosacral" part. Parasympathetic innervation to most of the gut comes from the "cranio-" half of that, i.e., the vagus nerve. The rest, to colon distal to the splenic flexure and to pelvic viscera, is from the "-sacral" half, via the pelvic splanchnic nerves. See also #7 below.)
Note: So far we have seen thoracic, lumbar, sacral, and pelvic splanchnic nerves. Remember that "splanchnic" really only means that they are going to viscera. It so happens that the first three emerge from sympathetic chain ganglia and carry sympathetic fibers, while the fourth has nothing to do with the sympathetic nervous system. If it helps, i.e. does not confuse you more, just remember that the splanchnic nerves come from the chain ganglia and carry sympathetic fibers, with the exception of the pelvic splanchnic nerves.
12. Trace the sympathetic and parasympathetic nerve supply to any pelvic organ, listing the location of the preganglionic cell body, the course of preganglionic fibers, the location of the postganglionic cell body, and the course of postganglionic fibers. (TG 8-18, 8-19, 8-20, 8-21)The sacral sympathetic trunk is slender, and often has 4 or fewer visible ganglia. The trunks lie on the anterior surface of the sacrum and the origin of piriformis, medial to the anterior sacral foramina, which have the large sacral ventral primary rami emerging laterally. The trunk has gray rami branching laterally to reach these sacral VPR's, and you may see very slender, hair-like sacral splanchnic nerves passing anteriorly onto the sides of the rectum to join the inferior hypogastric plexus.
13. Trace the skeletal and ligamentous boundaries of the perineum, and define the anal and urogenital triangles. (W&B 519, N 379A, 379B, TG 6-24A, 6-24B)Sympathetic: The preganglionic cell body is located in the lateral horn of the spinal cord in the thoracolumbar region. Axon travels out of the cord via the spinal nerve to the sympathetic chain ganglion. In the lumbar region, some of the nerves will synapse there and either travel down the chain to the pelvis or out via the lumbar splanchnic nerves. In the former case, they leave the chain in the pelvis, via a sacral splanchnic nerve, to reach the hypogastric plexus. In the latter case, they may reach the hypogastric plexus (the long way) via the superior hypogastric plexus and hypogastric nerves.
Parasympathetic: The preganglionic cell body is located in the lateral horn of the spinal cord in the sacral region. Axon travels out of the spinal cord via S2, S3, or S4 spinal nerves. These give off pelvic splanchnic nerves, which reach the hypogastric plexus. From here the neurons travel to their target, usually synapsing with a postganglionic neuron within the tissue of the target organ.
14. Describe the position and boundaries of the ischioanal fossa. (W&B 531-532)Officially, the perineum is the outlet of the pelvis. (Used more loosely, it can refer to the area of skin between the anus and the posterior part of the external genitalia.) It is diamond-shaped, and can therefore be divided into two isosceles triangles by a line drawn between the ischial tuberosities. The anterior, or urogenital triangle has as its apex the pubic symphysis, with the ischiopubic rami as equal sides, and our imaginary line as the base. The posterior, or anal triangle is upside-down, with our line again as the base, the sacrotuberal ligaments as the equal sides, and the coccyx as the apex. (peri + inan ("to empty out" in Greek))
You really need to think about this in 3-D because, although drawn two-dimensionally from an inferior point of view it looks like the coccyx, anus, vagina, and pubic symphysis are all coplanar, they are not.
15. Describe the structure, contents, and course of the pudendal canal. (W&B 524-526, N 404, 405, 411, 413, TG 6-28A, 6-28B)The ischioanal fossa lies lateral to the anal canal and inferior to the pelvic diaphragm. Its boundaries are as follows:
- Superomedial: pelvic diaphragm (anterior recess extends superior or deep to the sphincter urethrae muscle)
- Medial: external anal sphincter muscle and anal canal
- Lateral: obturator internus fascia and ischial tuberosity
- Posterolateral: sacrotuberous ligament and gluteus maximus muscle (posterior recess extends superior to the gluteus maximus muscle)
16. Differentiate between the internal and external anal sphincters in structure and function. (W&B 530, 537, N 391A, 391B, 392, 393, TG 6-15A, 6-15B, 6-16)The pudendal canal extends from the lesser sciatic foramen, where its contents enter the perineum, to the posterior edge of the perineal membrane. It contains the internal pudendal artery, internal pudendal vein, and the pudendal nerve.
- internal anal sphincter muscle: involuntary. It surrounds the superior 2/3 of anal canal. The internal anal sphincter muscle is a thickening of circular muscle that has parasympathetic innervation. It is contracted most of the time to prevent leakage of fluid and/or feces.
- external anal sphincter muscle: voluntary. It surrounds the superior 2/3 of anal canal as well, wrapped around the internal anal sphincter muscle. It constricts anal canal, but can be relaxed on command for the purpose of defecation.
Questions and Answers:
A1. Note the difference between male and female in the subpubic angle, the angle formed by the subpubic arch. What are other sex differences in the pelvic skeleton? (W&B 571-573, N 354, TG 6-05A, 6-05B, 6-05CD, 6-05EF)A2. Define the rectum. (N 393, 394, TG 6-08A, 6-08B, 6-15A, 6-15B, 6-15C, 6-16)
Structure/Section Female Male pelvic inlet oval and rounded heart-shaped pelvic outlet large small pubic arch and subpubic angle wide narrow iliac wings flared less flared A3. Define and note the flexure between rectum and anal canal. What muscle assists in maintaining this flexure? (N 393, TG 6-08A, 6-08B, 6-15A, 6-15B, 6-15C, 6-16)The rectum begins where the peritoneal investment of the sigmoid ends, at approximately the level of S3. It curves into the pelvic diaphragm, dilating just above the pelvic diaphragm as the rectal ampulla, and ends four centimeters below and in front of the coccyx. It continues as the anal canal after piercing the pelvic diaphragm. The rectum is about twelve centimeters long altogether. Its anterior surface contacts the vagina in females or the prostate gland in males.
A4. In the mucosa, define the anal columns and the pectinate line. What is their significance? (N 393, TG 6-16)The anterior flexure at the anorectal junction is held by the sling of the puborectalis portion of the levator ani muscle, which passes posteriorly around the anorectal junction.
A5. Locate the sympathetic trunk entering the pelvis along the medial border of the pelvic sacral foramina. Note number of ganglia, gray rami communcantes, and sacral splanchnic nerves. (N 410, 412, TG 8-18, 8-20)See #8 above.
Both sympathetic trunks descend on the anterior surface of the sacrum in the extraperitoneal connective tissue. There are usually four ganglia in the sacral region, one opposite the upper three sacral segments and one beneath the fourth and fifth segments of the sacrum. The two trunks typically unite over the coccyx to form the "ganglion impar". Sacral splanchnic nerves are slender fibers leaving the anterior surface of the sacral sympathetic trunk ganglia to enter the inferior hypogastric plexus on the sides of the rectum. Gray rami communicantes also leave the lateral side of the sacral sympathetic trunk to reach the sacral ventral primary rami as they emerge from the anterior sacral foramina.A6. How many pelvic splanchnic nerves are there? (N 410, 412, TG 8-19, 8-21)The pelvic splanchnic nerves represent the sacral portion of the craniosacral outflow or parasympathetic portion of the autonomic nervous system. The pelvic splanchnic nerves spring from the ventral rami of the second, third, and fourth sacral nerves. The contribution from the third sacral nerve is usually the largest. From three to ten strands of nerves pass forward and become incorporated into the inferior hypogastric plexus.A7. What is the puborectalis muscle? What is its significance? (N 367A, 367B, 368, 369, 370, TG 6-21A, 6-21B, 6-22, 6-23A, 6-23B)The puborectalis muscle is the most medial portion of the levator ani muscle. It passes around the terminal rectum to form the puborectal sling, which kinks the anorectal junction forward to assist in maintaining fecal continence. This muscle marks the transition from rectum to anus.A8. Define the urogenital hiatus. What does it transmit? (N 367A, 367B, 368, 369, 370, TG 6-21A, 6-21B, 6-22, 6-23A, 6-23B)The passage (transmission) of the urethra/vagina and anus through the pelvis requires a separation of the two halves of the pelvic diaphram in front of the rectum. This is the urogenital hiatus.